Problèmes oculaires
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Toni Hazell, MRCGPLast updated 10 Dec 2024
Répond aux besoins du patient lignes directrices éditoriales
- TéléchargerTélécharger
- Partager
- Langue
- Discussion
Dans cette série :Conjonctivite infectieuseConjonctivite allergiqueSécheresse oculaireEpisclérite et sclériteUvéiteHémorragie sous-conjonctivale
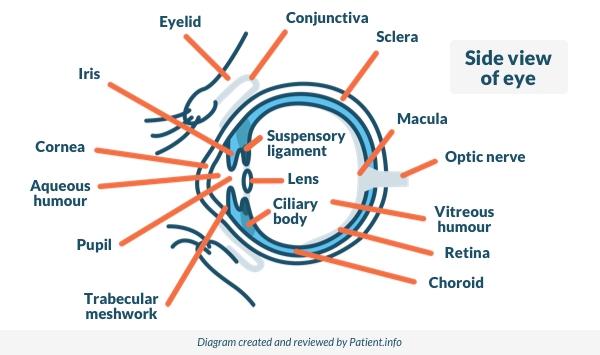
Eye problems range from everyday irritations to serious internal conditions. This leaflet contains a list of conditions which affect the eye, grouped together by the part of the eye which is affected or involved.
Dans cet article :
Points clés
There are many eye problems that can affect different parts of the eye, from surface issues such as pink eye and dryness to deeper issues such as uveitis or scleritis.
Signs of eye problems include redness, discomfort, blurred vision, and excessive tearing.
Treatment depends on the eye problem but options may include medications, lifestyle adjustments, or surgery.
Regular eye exams, proper hygiene, protection from irritants, and managing underlying health conditions can reduce the risk of having problems with your eyes.
Voir le dépliant intitulé Anatomie de l'œil pour plus de détails sur la structure de l'œil.
Poursuivre la lecture ci-dessous
Eye surface conditions: conjunctiva, cornea and sclera
La conjonctive est la partie claire et antérieure de l'œil qui recouvre le blanc de l'œil et le dessous des paupières. Les affections de la conjonctive n'ont généralement pas d'incidence directe sur la vision, car la lumière traverse la pupille et pénètre dans l'œil sans passer par la conjonctive.
La partie de l'œil en forme de disque transparent située au-dessus de la pupille et de l'iris est la cornée. Elle constitue la première partie du processus de focalisation d'une image sur le fond de l'œil. Les problèmes affectant la cornée sont donc susceptibles d'affecter la vision. La cornée étant très sensible, les problèmes qui l'affectent sont généralement douloureux.
Vue latérale de l'œil
Conjonctivite
Conjunctivitis is inflammation or infection of the surface layer of the eye (the conjunctiva). Conjunctivitis does not normally affect the vision, other than to make things slightly blurry due to watering or discharge over the eyes.
The patient has red itchy eyes, which may be sticky if the eyes are infected. See the separate leaflets called Allergic conjunctivitis and Infective conjunctivitis for more details.
Syndrome de Sjögren
Sjögren's syndrome is an autoimmune disease which most commonly causes dry eyes and mouth. It can also affect other organs including lungs, kidneys, skin and the nervous system. See the separate leaflet called Sjögren's syndrome.
Hémorragie sous-conjonctivale
This is a common cause of painless red eye, which looks very alarming. It is caused by a small bleed from one of the tiny blood vessels behind the conjunctiva. It can look alarming but it usually causes no symptoms and is usually harmless. Rarely, it can be associated with high blood pressure (hypertension). See the separate leaflet called Subconjunctival haemorrhage.
Episclérite et sclérite
Episcleritis and scleritis are inflammatory conditions which affect the eye. Both cause redness but scleritis is much more serious than episcleritis. Episcleritis causes redness with discomfort and irritation but without other significant symptoms. Scleritis affects the sclera and, sometimes, the deeper tissues of the eye. See the separate leaflet called Episcleritis and scleritis.
Ptérygion
A pterygium is a raised, yellowish, wedge-shaped thickening on the white part of the eye, which can occasionally spread over the cornea, obstructing vision. It is painless (although it can cause irritation, eye discomfort or dryness).
Pterygium occurs as a reaction by the eyes to being exposed to wind, dryness, dust and sunshine (solar radiation). It is particularly common in those who have lived in hot climates. It is sometimes called 'surfer's eye' or farmer's eye, as it is common in those who spend a lot of time outdoors where there are high levels of solar radiation.
It can be treated by surgery (either for cosmetic reasons or because it is starting to block vision) but often comes back; if it is not causing problems then nothing needs to be done. Sunglasses and artificial tears help prevent this.
Pinguecula
This yellow-white thickening of the sclera is common over the age of 40 years. It is caused by ultraviolet (UV) exposure, which leads to degenerative changes in the sclera. Small yellow-white deposits occur at the 3 o'clock or 9 o'clock positions on the eye. Because the surface is raised, the tear film may be interrupted, causing a loss of lubrication of the eye over the pinguecula, leading to pingueculitis.
This condition is similar to pterygium, except that only the conjunctiva is involved, and it forms a bump rather than a wedge-shaped growth. They are occasionally removed on cosmetic grounds and a pinguecula can develop into a pterygium. If it is not causing problems then nothing needs to be done.
Corps étrangers - quelque chose dans l'œil
If you get something in your eye then your eye will water and blink and will feel very uncomfortable. Foreign bodies which sit on the eye don't normally damage vision. However, objects which penetrate the eye and active chemicals which damage the surface (such as acids, alkalis and plaster dust) may do so, sometimes permanently.
Corneal Injury
Injury to the cornea may result in scarring, which can affect vision.
Infection de la cornée
Inflammation of the cornea is called keratitis and may be caused by various organisms, including germs such as bacteria and viruses. Viruses are the most common cause. See the separate leaflets called Shingles (Herpes zoster), Eye infection (Herpes simplex) and Visual problems (Blurred vision).
Les maladies auto-immunes, telles que la polyarthrite rhumatoïde, la maladie de Crohn et la spondylarthrite ankylosante, peuvent provoquer une kératite inflammatoire.
Allergic and inflammatory conditions of the cornea
Allergies affecting the eye may affect the cornea, with pollen as the most common allergen. Other allergens include medications, animal hair and cosmetics, such as mascara and face creams. See the separate leaflet called Allergic conjunctivitis.
Dry eyes and exposure keratitis
Dry eye syndrome (also known as keratoconjunctivitis sicca, or simply dry eyes) occurs when there is a problem with the tear film that normally keeps the eye moist and lubricated. See the separate leaflet called Dry eyes.
When the cornea dries out it may become irritated and inflamed, a condition called exposure keratitis. This can be caused by problems with tear production. Other causes include inability to close the eyelids properly, as in the facial nerve weakness seen in Bell's palsy.
Arc eye and snow blindness
Photokeratitis is sunburn of the cornea, usually noticed several hours after exposure to the sun. Snow blindness is the type of photokeratitis common in mountaineers and skiers who forget their sunglasses. Arc eye is a similar condition from exposure to the bright light of an arc lamp. See the separate leaflet called Visual problems.
Abnormalities of corneal size and shape
Keratoconus is an abnormally thin, curved cornea. It impairs vision and is treated with lenses and later contact lenses. Both help vision and protect the thinned eye surface. Corneal transplantation may be needed.
Astigmatism is a condition in which the corneal shape is slightly rugby ball-shaped rather than truly spherical, so that the focus of the eye is uneven. It is most commonly treated with corrective spectacles and contact lenses.
Corneal dystrophies
These are a group of progressive conditions which cause a build-up of cloudy material in the cornea. Most are inherited conditions, most affect both eyes and most progress only gradually. Some can affect vision, while others do not.
Poursuivre la lecture ci-dessous
Uveal eye conditions: iris, ciliary body and choroid
La partie colorée de l'œil s'appelle l'iris. L'iris est composé de fibres musculaires qui aident à contrôler la taille de la pupille. Le corps ciliaire est un petit muscle en forme d'anneau qui se trouve derrière l'iris et qui aide l'œil à faire la mise au point. La choroïde est la couche de tissu située entre la rétine et la sclérotique. Elle contient des vaisseaux sanguins et un pigment qui absorbe l'excès de lumière.
Uvéite antérieure
Uveitis is a general term describing inflammation of the part of the eye called the uveal tract, which consists of the iris, ciliary body and choroid. Anterior uveitis is the term for inflammation which affects the front (anterior) part of the uveal tract. It is the most common type of uveitis and the most painful. See the separate leaflet called Uveitis.
Aniridia
Aniridia is the absence of the iris, usually involving both eyes. It can be genetic, present from birth or caused by an injury. Most affected people have abnormalities further inside the eye and therefore often have severe visual impairment.
Larmoiement
Watering eyes can occur at any age but are most common in young babies and in people over the age of 60. It can occur in one or both eyes. See the separate leaflet called Watering eyes (Epiphora).
Iris heterochromia and anisocoria
Heterochromia is the term used when a person's two irises are different colours, sometimes partially and sometimes completely. It can be a lifelong condition due to the person's genetic makeup. However, it can also be caused by the use (in just one eye) of certain medications which affect eye colour, or can be the result of injury to the iris.
Iris heterochromia is easily confused with anisocoria. In anisocoria one pupil does not react to light in the same way as the other one, so that the pupils are of unequal sizes and the eye with the bigger pupil appears darker.
Eye fluid and drainage conditions: the ciliary body and trabecular meshwork
Le corps ciliaire est une partie de l'œil qui comprend les éléments suivants :
Le muscle ciliaire (qui modifie la forme de la pupille en modifiant la forme de l'iris).
L'épithélium ciliaire, qui produit l'humeur aqueuse. Il s'agit du liquide qui remplit l'avant de l'œil. L'humeur aqueuse est produite en continu. Elle circule dans la partie antérieure de l'œil et s'évacue par une zone appelée réseau trabéculaire, près de la base de l'iris.
Les problèmes de production et de drainage du liquide oculaire peuvent entraîner une augmentation de la pression à l'intérieur de l'œil (appelée pression hydrostatique) et différents types de glaucome. La raison sous-jacente du développement du problème n'est généralement pas claire. Toutefois, les affections inflammatoires de l'œil, les lésions oculaires et les médicaments à base de stéroïdes figurent parmi les causes connues.
Acute angle-closure glaucoma (AACG)
AACG (often just called acute glaucoma) occurs when the flow of aqueous humour out of the eye through the trabecular meshwork is blocked. Pressure inside the eye then becomes too high very quickly. If it is not treated quickly, it can lead to permanent loss of vision. See the separate leaflet called Acute angle-closure glaucoma.
Chronic open-angle glaucoma (COAG)
COAG (often just called glaucoma) occurs when there is a partial blockage within the trabecular meshwork. This restricts drainage and leads to a build-up of pressure. The increased pressure in the eye can damage eye nerve fibres and may affect vision. See the separate leaflet called Chronic open-angle glaucoma.
Ocular hypertension
In both types of glaucoma the pressure in the eye is increased. In AACG this causes pain and loss of vision. In COAG it causes no pain and a gradual loss of vision. However, the pressure in the eyeball is raised in both conditions.
Ocular hypertension is a condition in which the pressure in the eyeball is raised but pain and gradual loss of vision do not occur. Ocular hypertension affects around 5 in 100 people over the age of 40 years. However, most do not go on to develop the vision changes of glaucoma (although their risk of developing it is increased). It may be that the nerves in the eyes of people who develop glaucoma are more sensitive to pressure than the nerves in the eyes of those who do not.
Normal-tension glaucoma
This is almost the opposite condition to ocular hypertension. In normal-tension glaucoma the pressure in the eyes is not raised above what eye specialists consider normal. However, damage to the nerves of the eye typical of glaucoma nevertheless occurs.
The cause is uncertain, but it is believed that in these patients the nerves of the eye are particularly sensitive to pressure changes. These nerves can therefore be damaged even at pressures which are not considered harmful in most people.
Poursuivre la lecture ci-dessous
Lens and focusing conditions
Le cristallin peut changer de forme grâce au corps ciliaire qui contient de fines fibres musculaires qui tirent sur lui. Selon l'angle de la lumière qui lui parvient, le cristallin devient plus ou moins incurvé (convexe). Cela modifie sa force et lui permet de focaliser correctement la lumière au fond de l'œil.
Erreurs de réfraction
Les problèmes de focalisation peuvent vous obliger à porter des lunettes ou des lentilles de contact pour voir clairement. Il existe quatre principaux types d'erreurs de réfraction :
La myopie. Voir le dépliant séparé intitulé Myopie.
Hypermétropie. Voir la fiche séparée intitulée Hypermétropie.
Erreur de réfraction due à une courbure inégale de la cornée (astigmatisme). Voir la fiche séparée intitulée Astigmatisme.
La presbytie, liée à l'âge. Voir le dépliant séparé intitulé Presbytie.
Les erreurs de réfraction sont généralement traitées par un opticien, plutôt que par un médecin, de sorte qu'une visite chez le généraliste n'est généralement pas appropriée.
Cataracte
La cataracte est une affection dans laquelle le cristallin de l'œil se trouble et affecte la vision. La cataracte survient le plus souvent chez les personnes âgées et se développe progressivement. Au début, elle peut n'avoir que peu ou pas d'effet sur la vision. Voir le dépliant séparé intitulé Cataractes.
Dislocation du cristallin (ectopie lentis)
L'ectopie lentis est un déplacement partiel ou complet du cristallin par rapport à sa position normale. Elle peut survenir à la suite d'un traumatisme (la cause la plus fréquente - généralement un coup direct sur l'œil, l'orbite ou la tête). Il peut également résulter d'une maladie oculaire ou d'une maladie affectant l'ensemble du corps (maladie systémique). En plus d'affecter la vision, cette affection peut provoquer un glaucome (voir ci-dessus).
Parmi les maladies oculaires associées à l'ectopie lentis figure le syndrome de Marfan. Chez environ la moitié des personnes atteintes du syndrome de Marfan, le cristallin est disloqué à la naissance ou se disloque avant l'âge adulte. Les personnes atteintes du syndrome de Marfan sont également plus sujettes au décollement de la rétine (voir ci-dessous), à la myopie et à la cataracte. Voir la fiche séparée sur le syndrome de Marfan.
Posterior chamber eye conditions: the vitreous
The globe of the eye needs to keep its shape so that light rays are focused accurately on to the retina. The posterior part the eye is therefore filled with a jelly-like substance called the vitreous humour (or sometimes, the vitreous body or just the vitreous).
It consists mainly of water, with some protein (collagen), hyaluronic acid and salt. It helps to keep the retina in place by pushing it against the choroid. It is lightly attached to the retina posteriorly.
Posterior uveitis and other forms of uveitis
Uveitis is inflammation of the tissues of the eye. It can be described as anterior, posterior or intermediate uveitis, or panuveitis. See the separate leaflet called Uveitis.
Hémorragie vitréenne
Vitreous haemorrhage occurs when blood leaks into the vitreous humour inside the eye, most commonly from blood vessels at the back of the eye. If the vitreous humour is clouded or filled with blood, vision will be impaired. This varies from a few 'floaters' and cloudiness of the vision through to the vision going completely dark. See the separate leaflet called Vitreous haemorrhage.
Décollement du vitré postérieur
The vitreous is lightly attached to the retina at the back by protein fibres. As we age, the vitreous shrinks and eventually tends to pull away from the retina and cause a vitreous detachment. The vitreous is already detached in about 75% of people aged over 65 years. Many will not have been aware of it.
However, if symptoms occur they are light flashes and floaters (dots, spots or wispy lace objects floating across the vision), which can also be symptoms of retinal detachment. The flashes tend to settle once the detachment is complete. See the separate leaflet called Flashes, floaters and haloes.
Back of the eye conditions: the retina and optic nerve
La rétine est une couche située à l'intérieur de l'arrière du globe oculaire. Elle contient des cellules nerveuses hautement spécialisées. Celles-ci convertissent la lumière qui y est focalisée en signaux électriques. Ceux-ci sont ensuite transmis par les nerfs optiques aux parties du cerveau qui traitent la vision et construisent l'image que nous voyons.
La macula se trouve près du centre de la rétine. La macula est une petite partie très sensible de la rétine. Elle est responsable de la vision centrale détaillée, celle que vous utilisez lorsque vous regardez directement quelque chose. Elle contient la fovéa, la zone de l'œil qui produit les images les plus nettes.
Retinal detachment (RD)
The retina is made up of two layers: an inner layer of light-sensitive 'seeing cells' (called rods and cones) and an outer layer of pigmented cells which nourish and support them. RD occurs when the inner layer of rods and cones is separated from the retinal pigment epithelium (RPE). Symptoms include flashing lights, 'floaters' and loss of vision. Retinal detachment is a medical emergency. See the separate leaflet called Retinal detachment.
Dégénérescence maculaire
The macula is the small area of the retina at the back of your eye and responsible for your central vision. Age-related macular degeneration (AMD, or ARMD) is the most common cause of severe sight problems in the developed world. It causes a gradual loss of central vision. See the separate leaflet called Age-related macular degeneration
'Colour blindness' (colour vision deficiency)
Colour vision deficiency means you are unable to see certain colours. It is usually an inherited (genetic) disorder and you have it from birth. Red-green colour vision deficiency is the most common form. The condition can be variable from mild to severe. Some patients have no colour vision at all (achromatopsia). See the separate leaflet called Colour vision deficiency (Colour blindness).
Rétinite pigmentaire
Retinitis pigmentosa is the term for several inherited diseases with a gradual deterioration of the light-sensitive cells of the retina. Symptoms often start in childhood with difficulty seeing in the dark. See the separate leaflet called Visual problems.
Dystrophie rétinienne
Retinal dystrophies are a group of inherited disorders which result in changes to the retina, which may affect vision; some people with this condition will become blind in their 30s, whereas others will retain vision into old age. See the separate leaflet called Visual problems.
Charles Bonnet syndrome (CBS)
CBS affects people who have experienced a sharp decline in their vision. CBS involves visual hallucinations. These seem to occur as the brain stops receiving information from the retina and starts to replace it with information from our own memory stores. See the separate leaflet called Charles Bonnet syndrome.
Névrite optique
Optic neuritis is caused by inflammation of the optic nerve in the eye. It can involve one or both eyes and it can be recurrent. It is painful, particularly on eye movements. It can cause blurred vision or loss of colour vision. See the separate leaflet called Visual problems.
Optic neuritis can sometimes be the first sign of multiple sclerosis (MS), a disorder of the brain and spinal cord. Optic neuritis is the first symptom of MS for around one in four people with MS. However, not all optic neuritis is due to MS. See the separate leaflet called Multiple sclerosis.
Occlusion de la veine rétinienne
Retinal vein occlusion occurs when one of the tiny retinal veins becomes blocked by a blood clot. It usually leads to a painless decrease in vision in one eye. See the separate leaflet called Retinal vein occlusion.
Occlusion de l'artère rétinienne
Retinal artery occlusion is a blockage of all or part of the blood supply to the retina because the retinal artery is blocked by a blood clot. Occasionally both eyes are affected but this occurs in fewer than 2 in 100 cases.
Tumours of the eye and optic nerve
Tumours in the eye principally occur in the middle and inner layers of the eye, particularly the retina and optic nerve. They are rare. However, they include melanoma (which typically affects the choroid layer and is usually a tumour of later life) and retinoblastoma.
Mélanome choroïdien
Choroidal melanoma arises from pigment cells in the choroid layer. It is the most common primary malignant eye tumour in adults. 98% of all cases occur in ethnically white races. Most often it has symptoms which don't show (it is asymptomatic) and is found on chance examination. It can occasionally cause visual loss or vitreous haemorrhage. The majority of patients are over 50 years of age.
Rétinoblastome
Retinoblastoma is the commonest cancerous (malignant) tumour of the eye. It accounts for 3% of all childhood cancers. Onset generally occurs between the third month of pregnancy and 4 years of age with very few diagnosed later than 5 years of age. Most cases affect one eye only. The most common signs are leukocoria (a white pupil noticed on flash photography or in dim lighting) and squint (strabismus). The management of retinoblastoma has improved tremendously and it is now a largely curable disease.
Choriorétinite
Chorioretinitis is infection or inflammation of the choroid and retina. The choroid is the pigmented, highly vascular layer of the globe of the eye whose main function is to nourish the outer layers of the retina. The effect on vision depends on the location and size of the damaged area. See the separate leaflet called Visual problems.
Retinopathy
The term retinopathy covers various disorders of the retina that can affect vision. Retinopathy is usually due to damage to the tiny blood vessels in the retina. This leads to oxygen shortage followed by the growth of tiny new blood vessels in a disorderly way, often into the eye. These can bleed and the retina may be permanently damaged.
Retinopathy is commonly caused by diabetes but is sometimes caused by other diseases such as very high blood pressure (hypertension). See the separate leaflets called Diabetic retinopathy and High blood pressure (Hypertension).
Une autre forme de rétinopathie est observée chez les grands prématurés (moins de 32 semaines de gestation) qui ont besoin d'une oxygénothérapie. Il s'agit de la principale cause de déficience visuelle évitable chez l'enfant dans les pays développés.
Atrophie optique
Optic atrophy is the loss of some or all of the nerve fibres in the optic nerve. It causes reduction in vision or loss of vision. This may be central vision or edge vision or both, depending on which fibres are lost.
Optic atrophy is the end result of many conditions which can damage the optic nerve. These include glaucoma, head injury, retinal vein occlusion, retinal artery occlusion and MS. However, it can also happen alone without obvious cause. Some cases may be inherited.
Whole eye conditions
Maladie oculaire thyroïdienne
In thyroid eye disease the muscles and fatty tissues within the eye socket (orbit) become inflamed and swollen. This results in the eyeball being pushed forward, affecting the movements of the eye. In severe cases vision may be affected. See the separate leaflet called Thyroid eye disease.
Albinisme
Albinism covers a group of inherited disorders in which there is shortage of melanin production. Melanin is the pigment that gives colour to our skin, hair and eyes. Visual problems are an important part of albinism. Melanin is reduced or absent where it is normally present in the eye, skin, hair and brain. This causes abnormal development of the nerve pathways needed for vision.
Severe nystagmus (jumping of the eyes, usually from side to side), light sensitivity, squint and reduced vision are common features. Contrary to common belief, the irises of patients with albinism are not pink. Instead it varies from a dull grey to blue and even brown (brown is common in ethnic groups with darker pigmentation).
Under certain lighting conditions there is a reddish or violet hue reflected through the iris from the retina and the eyes can appear red. Not all types of albinism result in very pale skin and hair.
Colobome
Coloboma is a defect or gap in the tissues of the eye, occurring during development in the womb. It can involve one or more of several parts of the eye, including the eyelid, cornea, iris, ciliary body, lens, retina, choroid and optic disc.
Coloboma is a rare condition and is sometimes associated with abnormally small eyes (microphthalmia). Not all colobomata affect vision. However, the condition is an important cause of childhood visual impairment. Worldwide, it causes around 1 in 20 cases of severe visual impairment in childhood.
Conditions de mouvement des yeux
Squint (strabismus)
Strabismus is a condition where the eyes do not look in the same direction. Whilst one eye looks forwards to focus on an object, the other eye turns either inwards, outwards, upwards or downwards. Most squints occur in young children. See the separate leaflet called Squint in children (Strabismus).
Nystagmus
Nystagmus is a symptom, rather than a diagnosis, in which there is a repetitive to-and-fro oscillation of the eyes outside the person's control. It usually affects both eyes, with one worse than the other.
Most nystagmus is present from an early age and is caused by abnormalities of visual development in childhood. This leads to sensory deprivation of the retina. Nystagmus which comes on after childhood is more often due to diseases of the balance organs. These include labyrinthitis and disorders of the brain such as MS, diabetic neuropathy and brain tumours.
Nystagmus is involuntary, meaning people with the condition cannot control their eyes. It improves slightly as a person reaches adulthood but worsens with tiredness and stress. Most people with nystagmus have visual difficulties because the eyes continually sweep over what they are viewing, making it impossible to obtain a clear image.
To see better, patients may turn their head and lock their eyes into what's called the 'null point'. This describes the head angle that makes the eyes move the least, to attempt to stabilise what they see. Nystagmus can occur as a short-term sign, for example in some conditions that cause a type of dizziness called vertigo.
Affections des paupières
Chalazion
A chalazion is a small (2-8 mm) fluid-filled swelling (cyst) in the eyelid. It is common and sometimes called a meibomian cyst or tarsal cyst. A chalazion is more common on the upper eyelid and can affect both eyes. It is not the same as a stye. See the separate leaflet called Chalazion.
Stye
A stye is a common painful eyelid problem, where a small infection forms at the base of an eyelash. It looks like a small yellow pus-filled spot. Vision is unaffected. See the separate leaflet called Stye.
Ectropion et entropion
When part or all of the lower eyelid turns outwards away from the eye, the condition is known as an ectropion. An entropion occurs where the eyelid turns towards the eye, causing the eyelashes to rub against the front of the eye (cornea). See the separate leaflets called Ectropion and Entropion.
Lagophthalmos
Lagophthalmos is the inability to close the eyelids completely. This leads to corneal exposure and dryness. The main cause is facial nerve paralysis. However, it can occur after trauma or eyelid surgery (cicatricial lagophthalmos) or during sleep (nocturnal lagophthalmos). The main cause is Bell's palsy.
Paralysie de Bell
Bell's palsy is the most common cause of sudden facial weakness (paralysis). It is due to a problem with the facial nerve. It may cause a watery or dry eye that will not close properly. See the separate leaflet called Bell's palsy.
Drooping eyelids
Drooping of the eyelid is called ptosis by doctors. It may affect one or both lids and there are many causes. People may comment that you look sleepy or tired.
Ptosis
Ptosis can be due to long-term contact lens wear, to eye trauma or surgery, or to simple ageing of the muscles of the eyelid. Less common causes of ptosis include diseases causing muscle weakness (such as myasthenia gravis and myotonic dystrophy) and conditions affecting the nerves to the eyelid.
Floppy eyelid syndrome
Floppy eyelid syndrome is a specific condition which tends to occur in obese men and is often associated with sleep apnoea and snoring. The loose lids tend to come apart during sleep, resulting in an exposed cornea.
Blépharite
Blepharitis means inflammation of the eyelids. It causes the eyes to feel sore and gritty. It can be a troublesome and recurring condition with no one-off cure. It can be associated with other skin conditions such as rosacea and seborrhoeic dermatitis. See the separate leaflet called Blepharitis.
Affections des cils
De nombreuses conditions peuvent affecter la croissance et l'apparence des cils :
Le trichiasis est un problème du bord de la paupière dans lequel les cils sont mal orientés et en contact avec la surface de l'œil (oculaire). Il est généralement causé par la cicatrisation des follicules des cils.
La polio est un blanchiment prématuré et localisé des cils et des sourcils.
La madarose est la perte de sourcils ou de cils. Elle est fréquente et se produit en association avec des affections touchant l'ensemble du corps (affections systémiques) et avec des affections localisées. Il s'agit notamment de
Une glande thyroïde trop active(hyperthyroïdie).
Une glande thyroïde insuffisamment active(hypothyroïdie).
Maladie auto-immune.
Vieillissement normal.
Infections des paupières.
Certains médicaments.
Affections générales affectant l'œil
De nombreuses affections dont les effets principaux se manifestent ailleurs dans le corps peuvent affecter l'œil, même si ce n'est pas toujours le cas. Il s'agit notamment de
Diabète sucré - peut provoquer une rétinopathie diabétique.
L'hypertension artérielle peut provoquer une rétinopathie hypertensive.
Un excès d'hormone de croissance(acromégalie) peut provoquer une atrophie optique.
Troubles inflammatoires - les troubles qui affectent particulièrement les articulations peuvent également enflammer l'œil, provoquant une sclérite ou une uvéite. Il s'agit notamment de
Polyarthrite rhumatoïde - peut provoquer une épisclérite, une sclérite et une sécheresse oculaire.
Lupus érythémateux disséminé - peut provoquer une sécheresse oculaire, une kératite et une sclérite, une vascularite rétinienne ou une neuropathie optique.
Spondylarthrite ankylosante - cause fréquente d'uvéite antérieure.
Arthrite réactive - peut provoquer une conjonctivite et une uvéite.
Maladie de Crohn et colite ulcéreuse - peut provoquer une uvéite, une kératite, une sécheresse oculaire et une épisclérite.
Sarcoïdose - peut provoquer une inflammation de la conjonctive et une uvéite postérieure.
Sclérose systémique - peut provoquer un resserrement des paupières.
Rhumatisme psoriasique - peut provoquer une uvéite, une conjonctivite, une kératite ou une sécheresse oculaire.
VIH/SIDA - de nombreux problèmes oculaires peuvent survenir en cas de SIDA, notamment des infections graves, l'uvéite, la rétinopathie, la choriorétinite et des anomalies de la pupille.
Syndrome de Gilbert - il s'agit d'une maladie dans laquelle le foie ne traite pas très bien la bilirubine. Elle est généralement inoffensive, bien qu'elle puisse occasionnellement provoquer un jaunissement de la peau et du blanc des yeux (jaunisse).
Vitamin A deficiency - vitamin A is important for healthy eyes. Severe deficiency may cause night blindness, corneal thinning and dryness and even retinal damage.
Questions fréquemment posées
What are the four most common eye problems?
The four most common eye problems are short-sightedness (myopia), long-sightedness (hyperopia), astigmatism, and presbyopia. These conditions affect how clearly you see and often require glasses or contact lenses to correct vision.
What is the most serious symptom with the eye?
The most serious eye symptoms include sudden vision loss, severe pain, flashes of light, or a sudden increase in floaters. These may indicate urgent conditions such as retinal detachment, acute glaucoma, or eye infection and require immediate medical attention.
Le Dr Mary Lowth est l'auteur ou l'auteur original de cette brochure.
Choix des patients pour Problèmes oculaires

Santé des yeux
Episclérite et sclérite
L'épisclérite et la sclérite sont des affections inflammatoires qui touchent l'œil. Toutes deux provoquent des rougeurs, mais la sclérite est beaucoup plus grave (et plus rare) que l'épisclérite.
par le Dr Doug McKechnie, MRCGP

Santé des yeux
Déficience de la vision des couleurs
Colour vision deficiency, also called colour blindness, is when you are unable to see certain colours. The most common form of the condition is red-green colour vision deficiency.
par le Dr Hayley Willacy, FRCGP
Autres lectures et références
- Asbell P, Messmer E, Chan C, et alDefining the needs and preferences of patients with dry eye disease (Définir les besoins et les préférences des patients souffrant de sécheresse oculaire). BMJ Open Ophthalmol. 2019 Dec 5;4(1):e000315. doi : 10.1136/bmjophth-2019-000315. eCollection 2019.
- Valikodath NG, Newman-Casey PA, Lee PP, et al.Agreement of Ocular Symptom Reporting Between Patient-Reported Outcomes and Medical Records (concordance des rapports sur les symptômes oculaires entre les résultats rapportés par les patients et les dossiers médicaux). JAMA Ophthalmol. 2017 Mar 1;135(3):225-231. doi : 10.1001/jamaophthalmol.2016.5551.
Poursuivre la lecture ci-dessous
Historique de l'article
Les informations contenues dans cette page sont rédigées et évaluées par des cliniciens qualifiés.
Prochaine révision prévue : 9 décembre 2027
10 Décembre 2024 | Dernière version

Demandez, partagez, connectez-vous.
Parcourez les discussions, posez des questions et partagez vos expériences sur des centaines de sujets liés à la santé.

Vous ne vous sentez pas bien ?
Évaluez gratuitement vos symptômes en ligne
Inscrivez-vous à la newsletter destinée aux patients
Votre dose hebdomadaire de conseils santé clairs et fiables, rédigés pour vous aider à vous sentir informé, confiant et maître de la situation.
En vous abonnant, vous acceptez notre politique de confidentialité. Vous pouvez vous désabonner à tout moment. Nous ne vendons jamais vos données.